Medically reviewed by Catherine Hansen, MD, OBGYN & Menopause specialist
Perimenopause is an important phase in a woman’s life, marking the transition from reproductive years to menopause. This natural biological process can occur anytime between the ages of 35 and 50, although it typically occurs in women in their 40s, and can last anywhere from a few months to several years. The timing and duration of perimenopause vary from woman to woman since we are all different and unique and our experiences are not always the same!
During perimenopause, the body undergoes hormonal changes that can cause a range of physical and emotional/cognitive symptoms. Understanding and recognizing symptoms of perimenopause is crucial for women to effectively manage this transitional phase and take control of their health. This informational guide will provide an in-depth overview of common perimenopausal symptoms and offer practical tips for managing them, so you can navigate this time with greater ease and confidence.
Common Perimenopause Symptoms
A woman can experience different symptoms during perimenopause as they vary for each individual. Here we present some of the most common ones divided by physical and cognitive.
Perimenopause Physical Symptoms
Irregular periods
As women approach perimenopause, their menstrual cycles may become irregular, with periods becoming shorter or longer, heavier or lighter, and more or less frequent. This is due to fluctuating levels of hormones, particularly estrogen, and progesterone, which regulate the menstrual cycle.
These changes can have a significant impact on daily life, causing anxiety about unpredictable periods, making it difficult to plan social events, and affecting sexual activity.
Hot flashes and night sweats
Hot flashes, also known as hot flushes and scientifically named vasomotor symptoms, are sudden intense feelings of heat that can cause sweating, flushing, and palpitations. They can last between 5 and 10 minutes and their frequency varies from woman to woman. Some may experience a few over a week and others may have over 10 very intense hot flashes per day. They can also occur at any time, causing discomfort and embarrassment in social situations. Night sweats are hot flashes that occur during sleep, leading to disrupted sleep patterns and fatigue.
Research shows that over 80% of women experience hot flashes during perimenopause. The cause of hot flashes and night sweats is not fully understood, but it is thought to be related to changes in the hypothalamus, which regulates body temperature.
Vaginal dryness
As you approach perimenopause, the levels of estrogen and progesterone hormones in your body may decrease, which can affect your vagina. This hormonal change can cause vaginal walls to become thinner, drier, and less elastic, and the external tissue may also decrease and thin out. As a result of these changes, women may feel discomfort, including irritation, itching, pain, or burning while performing everyday activities. Sexual activity can also become less enjoyable, potentially causing pain and discomfort and leading to decreased libido.
Bone density loss
During the menopause transition, women are at an increased risk of osteoporosis and fractures due to decreased estrogen levels in their bodies. Estrogen plays a crucial role in maintaining bone density, and as it declines during perimenopause can increase the risk of bone mass loss and osteoporosis.
Fatigue
Some women reported feeling persistent tiredness and lack of energy during perimenopause, affecting daily activities. Hormonal imbalances, stress, and anxiety can disrupt sleep patterns, leading to fatigue, impairment in memory, and decreased productivity.
Hair loss
As women approach perimenopause, their estrogen levels begin to decline, which can have an impact on hair growth and health. Estrogen plays a major role in regulating the hair growth cycle, and a drop in estrogen levels can cause hair strands to become thinner and shed more frequently. Additionally, during perimenopause, androgen or male hormone levels may increase, causing hair shafts to shrink in diameter, further contributing to a decrease in hair volume. These hormones can also stunt hair growth, leading to overall thinning and lack of volume.
Urinary incontinence
Involuntary leakage of urine can be categorized into two main forms, overactive bladder and stress incontinence. Overactive bladder is related to anything that irritates the bladder wall such as caffeine, alcohol, smoking, medications and certain foods (eg. spicy or acidic). Avoiding these irritants can reduce or eliminate symptoms. Women may be more prone to overactive bladder during perimenopause or menopause due to the lack of estrogen that protects the bladder wall.
The other type of incontinence is called stress incontinence and is related to laxity in the pelvic floor at the bladder neck. It is noted mostly with coughing, sneezing, or laughing. Stress incontinence may be impacted by hormones because of the impact of estrogen on the elasticity of the bladder, bladder neck and pelvic floor tissues. While changes during perimenopause may contribute to urine leakage in middle-aged women, it’s not the only factor that can cause this issue. Other factors that may have a role include the natural weakening of muscles due to age, pelvic floor injuries after giving birth, and underlying conditions like diabetes, multiple sclerosis, or Parkinson’s disease. Also, certain medications like antidepressants or painkillers, sedentary lifestyles, and obesity can be factors that contribute to difficulties with bladder control. Understanding these various factors can help women take steps to address urinary incontinence and improve their overall health and well-being.
Perimenopause Cognitive Symptoms
Mood swings
Perimenopause can also cause mood swings, anger, irritability, anxiety, and depression. This can be due to the fluctuating levels of hormones, particularly estrogen, which can affect neurotransmitters in the brain. According to the American College of Obstetricians and Gynecology 4 out of 10 women experience mood changes during perimenopause. These changes can impact daily life, causing difficulty concentrating, low energy, and reduced productivity.
Anxiety
During perimenopause, the hormone receptors in your brain may start to decrease, leading to disruptions in the biochemical activity that regulates mood. This can result in changes in mental health, including an increase in anxiety symptoms like irritability, nervousness, tension, and racing heart. While occasional feelings of anxiety are normal during this time, frequent panic attacks or high levels of anxiety could be a sign of a more serious condition and should be evaluated by a medical professional. Symptoms of panic disorder may include shortness of breath, chest pain, dizziness, heart palpitations, and feelings of losing control. It’s worth noting that the unsettling feelings that sometimes accompany hot flashes can mimic or trigger panic attacks.
Sleep disturbances
Some women may experience difficulty falling asleep, staying asleep, or poor sleep quality. Night sweats and hormonal fluctuations can disrupt sleep patterns, leading to insomnia and daytime sleepiness.
Decreased libido
Decreased libido translates to reduced sexual desire or interest. Hormonal changes as seen before can affect libido and sexual function, leading to a decrease in sexual desire and satisfaction in midlife.
Memory problems
Cognitive issues such as difficulty with concentration, forgetfulness, or mental fog are also related to hormonal changes. These changes can affect cognitive function and memory, leading to difficulties with concentration and memory recall. A study has shown that perimenopausal women report more memory problems than premenopausal women (women that are neither perimenopausal, menopausal, nor postmenopausal).
What causes perimenopause symptoms?
The primary cause of perimenopausal symptoms is the decline in estrogen levels. During perimenopause, the ovaries gradually produce less estrogen, which is a hormone that plays a crucial role in regulating the menstrual cycle and maintaining various bodily functions. As estrogen levels decrease, it can disrupt the delicate balance of hormones in the body, leading to a range of symptoms, some of which we discussed previously.
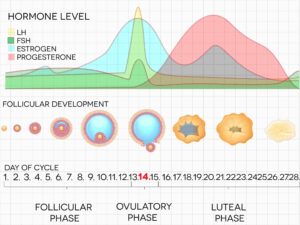
Let’s understand how estrogen works and its function in a woman’s cycle. Estrogen levels in women’s bodies are mainly controlled by two hormones called follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FSH signals the follicles, which are sacs in the ovaries containing the eggs, to produce estrogen. When the level of estrogen reaches a certain point, the hypothalamus in the brain tells the pituitary gland to stop producing FSH and instead release LH. Then, the ovary releases the egg from its follicle, which is called ovulation. The leftover follicle produces both estrogen and progesterone, preparing for a possible pregnancy. As the levels of these hormones increase, the levels of FSH and LH decrease, this is called a feedback loop. If pregnancy does not occur, progesterone falls, menstruation takes place, and the cycle starts again.
Since perimenopause is the transition phase to menopause when a woman’s body no longer needs to produce eggs for fertilization, we have a deeper understanding about why the estrogen levels start to fall as the body prepares to enter menopause.
Hormonal fluctuations during perimenopause can vary from woman to woman, and the severity and duration of symptoms can also differ. Some women may experience mild symptoms that are easily manageable, while others may experience more severe symptoms that significantly impact their quality of life.
It’s important to note that while hormonal changes are the primary cause of perimenopause symptoms, other factors can also contribute to the overall experience. These include:
- Aging: As women age, the number of follicles in the ovaries decreases, leading to a decline in the production of estrogen. This natural aging process is the primary cause of perimenopause.
- Genetics: The timing and severity of symptoms experienced during menopause can be influenced by genetic factors. If your mother or sister experienced early menopause or had severe symptoms, you may be more likely to experience similar patterns.
- Lifestyle factors: Certain lifestyle factors can influence the onset and severity of symptoms. Factors such as smoking, excessive alcohol consumption, a sedentary lifestyle, and a poor diet can exacerbate symptoms and increase the risk of complications.
- Medical conditions: Certain medical conditions or treatments can also contribute to symptoms. For example, women who have undergone cancer treatments, such as chemotherapy or radiation therapy, may experience premature or sudden menopause.
Lastly, there are additional psychological factors such as anxiety and depression.
Understanding the underlying causes of perimenopausal symptoms is essential for developing effective management strategies and getting the right support you need. By addressing hormonal imbalances, managing lifestyle factors, and seeking appropriate medical treatment when necessary, women can effectively navigate through perimenopause and minimize the impact of symptoms on their daily lives.
How to Manage Perimenopausal Symptoms
While perimenopause symptoms can be challenging, there are practical steps women can take to manage them:
- Prioritize self-care: Engage in stress-reducing activities, practice mindfulness, and engage in hobbies or activities that bring joy. Taking care of one’s mental and emotional well-being is essential during this transitional phase.
- Maintain a healthy lifestyle: Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Regular exercise can help manage weight, improve mood, and promote better sleep. Prioritize sleep hygiene by creating a relaxing bedtime routine and ensuring a comfortable sleep environment.
- Seek professional help: Consult a physician for accurate diagnosis and personalized treatment options. Our team of healthcare professionals specializes in perimenopause management and can provide accurate diagnosis and personalized treatment options tailored to your specific health history and needs. Through our convenient online platform, you can easily access medical treatment such as birth control and menopausal hormone therapy targeted to your symptoms and needs.
Self-Care and Support
Self-care is crucial during perimenopause. Women should prioritize their well-being by practicing relaxation techniques, seeking support from professionals, friends, and family, and considering joining support groups. Connecting with others who are going through similar experiences can provide valuable emotional support and helpful tips for managing symptoms (if you are interested in gathering with other women in a safe, supportive space, have a look at the Empowered Women’s Circle, led by Pandia Health’s Lead Physician on Menopause, Dr. Catherine Hansen.
At Pandia Health, we understand that managing the symptoms of perimenopause can be challenging. That’s why we offer convenient and personalized, perimenopause treatment and telemedicine to help you find relief and regain control of your life. With our expert online doctor service we aim to provide you with effective treatment options delivered right to your doorstep, ensuring a hassle-free experience. Join us today to start effectively managing your perimenopause symptoms and take control of your health and your life!
Disclaimer: This article is for general informational purposes and is NOT a substitute for professional medical advice. Always seek the advice of your healthcare provider before starting or changing birth control.